Abstract
Objective
For RSI, Nondepolarizing NMB has gradually replaced succinylcholine. However, its long-duration paralysis effect may prolong the vulnerable status of critically ill patients after intubation.
Does the incidence of post-intubation cardiac arrest differ between depolarizing and nondepolarizing NMBs?
Methods
A retrospective analysis of acute respiratory failure patients who received RSI in a university hospital in the past 12 years.
Results
Demographic data:
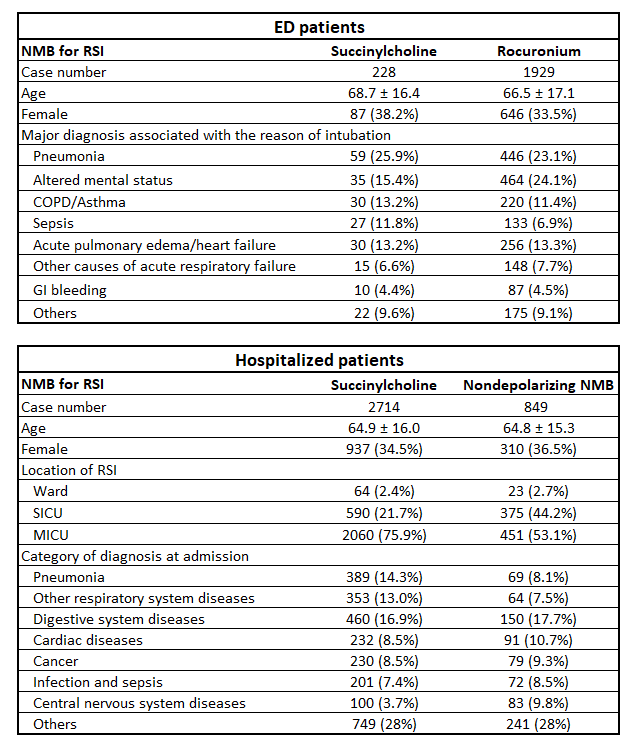
Outcomes:
| Succinylcholine | Nondepolarizing NMBs | P value | |
| ED cases, N | 228 | 1929 | |
| Status of leaving ER | 0.33 | ||
| Expired | 4 (1.8%) | 55 (2.9%) | |
| ICU admission | 224 (98.2%) | 1874 (97.1%) | |
| Hospitalized cases, N | 2714 | 849 | |
| CPR within 6 hours after RSI | 185 (6.8%) | 43 (5.1%) | 0.069 |
| All cases, N | 2942 | 2778 | |
| Combined cardiac arrest events | 189 (6.4%) | 98 (3.5%) | <0.05 |
Conclusion
After RSI, the mortality at ED and the incidence of CPR events within 6 hours during hospitalized patients are similar between different choices of NMBs. The combined data show that succinylcholine is associated with higher cardiac arrest events.