Abstract
Background: Lung volumes vary markedly at a given FEV1 in COPD. The impact of these inter-subject differences on relevant clinical outcomes remains unclear.
Aim: To investigate the relationship between resting lung volumes with exertional dyspnea and exercise tolerance in patients with mild-to-very severe COPD.
Methods: 345 patients (193 ?) with measurements of "static" lung volumes and incremental exercise testing Lung volumes beyond the statistical limits of normal (GLI equations) established abnormality.
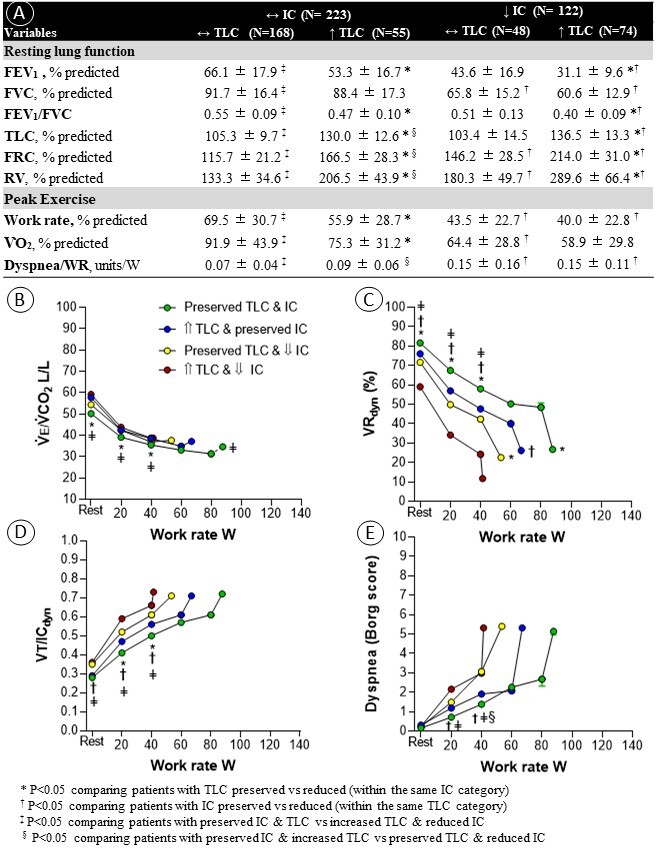
Results: Four phenotypes were identified: patients with or without low volumes for tidal expansion (preserved (?) or low (?) inspiratory capacity (IC)), each group divided into those with ? or high (?) total lung capacity (TLC) (lung overdistension). Lung overdistention was associated with higher functional residual capacity and residual volume in each IC category (A). Regardless of IC, those with ? TLC showed lower submaximal ventilatory reserves (VRdyn) (C) and higher operating lung volumes (D). Patients showing ? IC had worse exercise capacity and dyspnoea; of note, however, ? TLC was associated with poorer exercise tolerance in patients with ? IC (p<0.05; A and E).
Conclusions: Measurements of ?static? lung volumes - particularly in the setting of preserved IC - enhance the physiological phenotyping of COPD, pointing out to more dyspnoeic and physically limited patients.