Abstract
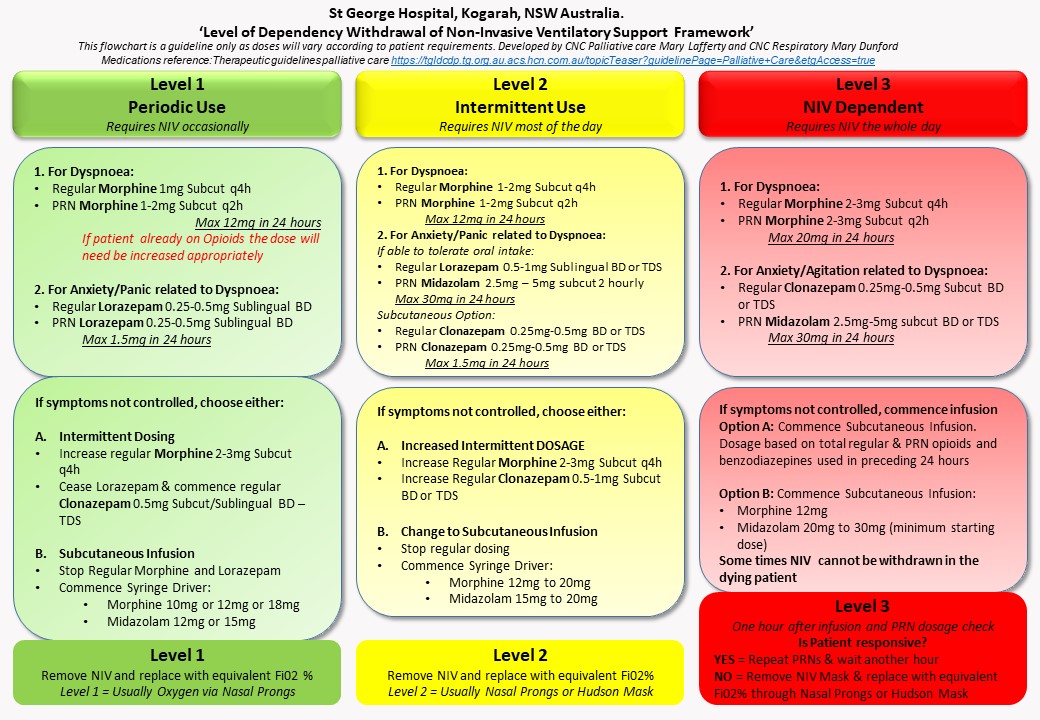
Background: Inconsistencies in medication dosages used when withdrawing non-invasive ventilatory support (NIVs) led to the development of a ?level of dependency withdrawal of NIVs framework? to promote consistent symptom management for end-of-life care (EOLC) in patients with respiratory failure. (Figure1)
Aim: Investigate the impact of the ?level of dependency withdrawal of NIVs framework? on symptom management in patients with respiratory failure.
Methods: Retrospective analysis of the impact of the framework was completed between 2015 and 2020 at a large teaching hospital in Sydney Australia. Respiratory symptoms of dyspnoea, anxiety, and agitation were collected and analysed.
Results: Data of 81 patients with a mean age of 76.3 years and 51 (63%) were male. Significantly fewer patients had agitation at death following the implementation of the framework (14%) compared to preintervention (42.1%) (OR 0.22, 95% CI 0.08, 0.65). There was a non-statistically significant reduction in dyspnoea and anxiety at death post-intervention. After the commencement of the framework, 71.6% of all patients were withdrawn from NIVs within 24 hours and 78% by the time of death.
Conclusion: Implementation of this framework has significantly reduced the burden of respiratory symptoms in this patient group during the withdrawal of NIVs in EOL.