Abstract
Background:
Risk stratification is important for optimized management in pulmonary arterial hypertension (PAH).
Objectives:
To assess the performance of risk stratification tools by adding variables specific to systemic sclerosis (SSc) to predict mortality.
Methods:
We included patients with SSc-PAH (according to the 2022 ESC/ERS Guidelines) from the EUSTAR registry from 2001-2022 (CP122). We applied:
A. 2022 ESC/ERS 3-strata: Variables graded 1-3 (low-high risk)
B. 2022 ESC/ERS 4-strata: Equals A, intermediate in two groups
C. COMPERA 2.0: Variables (WHO-FC, 6MWD, proBNP) graded 1-4 (low-high risk)
D. REVEAL Lite 2: Three groups based on six weighted variables
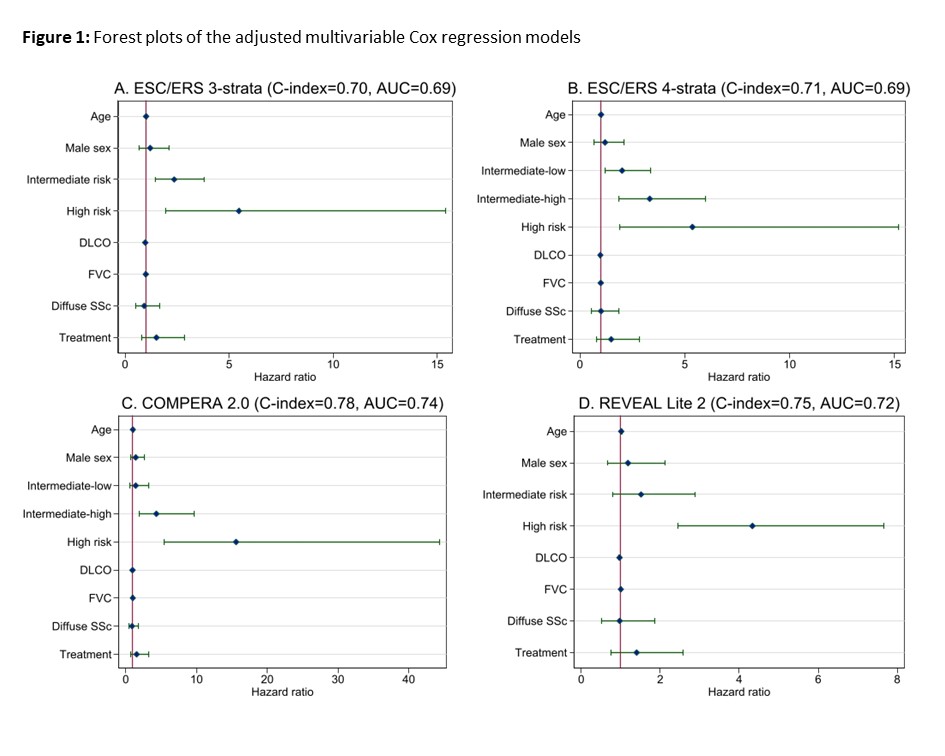
We performed Cox regression adjusted for age, sex, DLCO, FVC, SSc subtype and PAH treatment. We compared the models using C-index and ROC analysis with area under the curve (AUC) with >0.7 defined as acceptable.
Results:
In 430 SSc-PAH patients only COMPERA 2.0 had acceptable predictive value in univariable analysis (C-index=0.73, AUC=0.71). When we adjusted for SSc-specific variables, all the models predicted mortality. Hazard ratios increased with higher risk scores (Fig. 1). COMPERA 2.0 was most accurate to predict mortality (Fig. 1C).
Conclusions:
In SSc-PAH, we suggest that the application of risk stratification tools at the time of PAH diagnosis should take SSc-specific variables into account. COMPERA 2.0 performs best and is easily applicable in clinical practice.