Abstract
Patients with chronic thromboembolic pulmonary hypertension (CTEPH) should be considered for a multimodal treatment approach: pulmonary endarterectomy (PEA), balloon pulmonary angioplasty (BPA) and medical therapy. We assessed long-term outcome for the UK national cohort between 2015-2022 when all 3 treatment options were available.
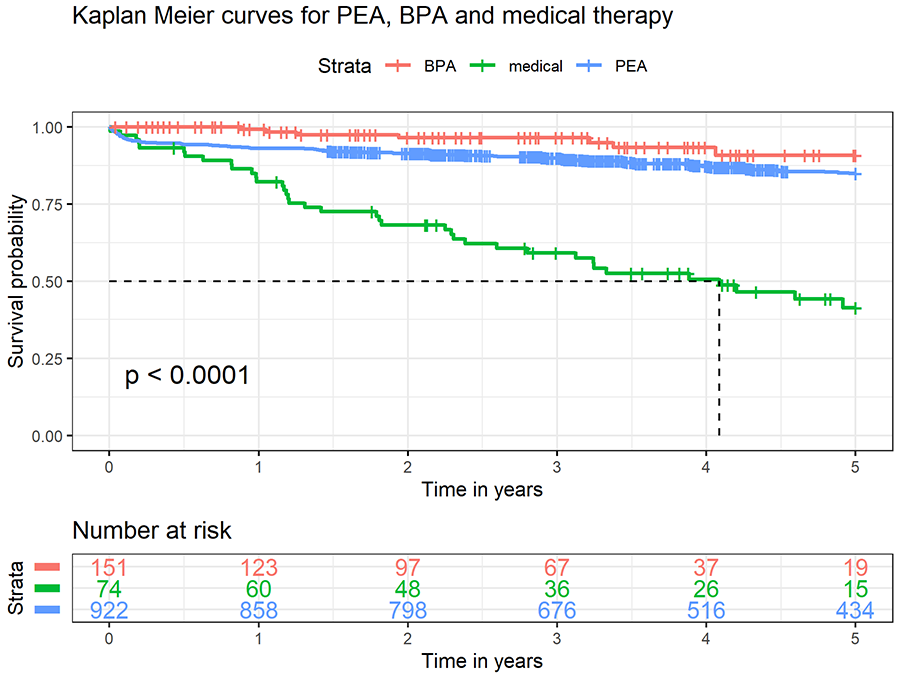
1147 patients underwent either PEA (national, n=922), BPA (national, n=151) or were treated with medical therapy only (single centre, n=74). Treatment modality was decided in a national CTEPH multidisciplinary team meeting (MDT) according to anatomical distribution of chronic clots and individual risks and benefits. Long-term survival after intervention or start of therapy was assessed by Kaplan-Meier and log-rank analysis.
Median age was significantly higher in the medical and BPA group compared to PEA (73 vs. 66 vs. 60 years, p <0.001). Median mean pulmonary artery pressure at baseline was 45 vs 41 vs 46 mmHg (p<0.001). 3-year survival probability for medical, BPA and PEA was 59, 96 and 90% respectively (log-rank, p<0.0001). For PEA, conditional survival from first follow-up showed no significant difference to BPA (95 vs 96%, p=0.98).
We observed excellent long-term survival for CTEPH patients undergoing PEA or BPA. However, the three treatment modalities are not interchangeable and decision making for each patient is dependent on an experienced MDT.