Abstract
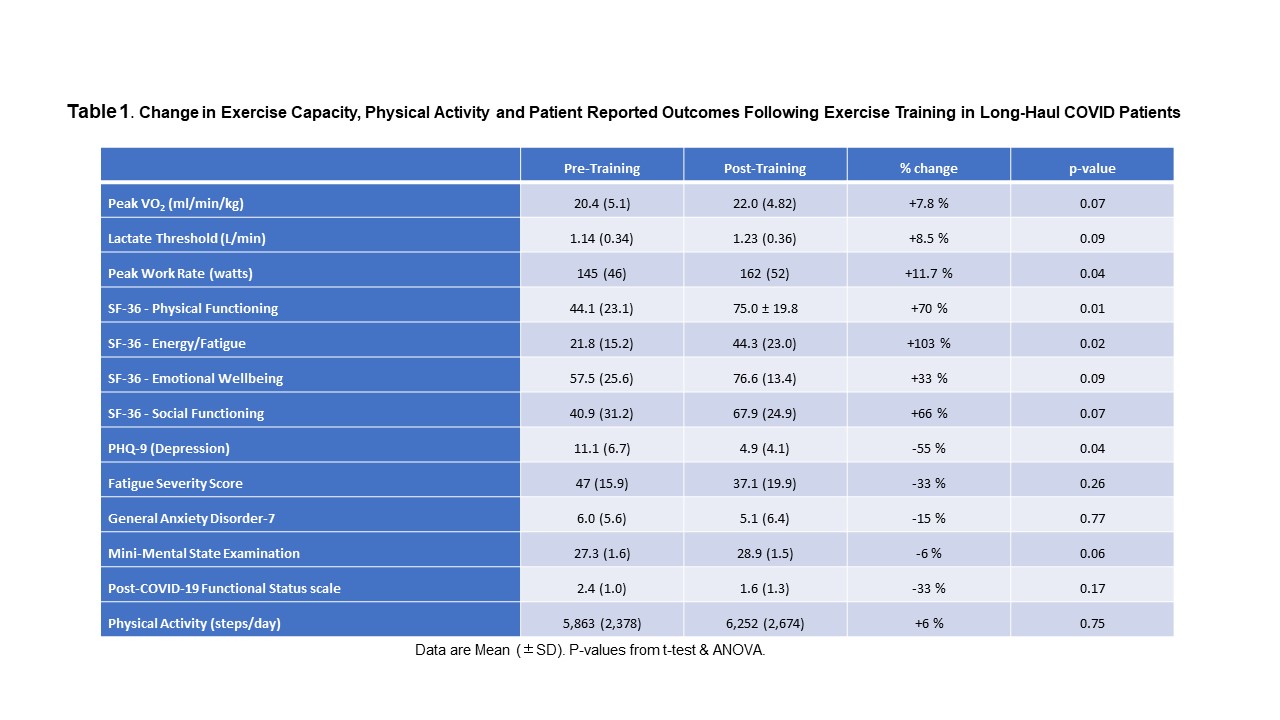
Aim Non-hospitalized Long-Haul COVID (LHC) patients without significant autonomic dysfunction were studied to determine tolerance/benefit from exercise training. Methods Effects of 10 weeks progressive aerobic interval exercise training were assessed (20 sessions). Pre- and post-training assessments: cardiopulmonary exercise testing; physical activity (triaxial accelerometry); questionnaires for quality of life, depression, fatigue, anxiety, mental state, post-covid functional status; and immunological measurements were investigated in 12 subjects (Table 1). Blood samples were collected at baseline and peak incremental exercise for immunophenotyping (flow cytometry). Results 12 participants were enrolled: (average age 52±11y, 46% female, BMI 43.7±7.7, 50% prior smokers, normal pulmonary function). 92% presented with fatigue and brain fog. Compliance with training was > 95%. Post-training improvements were found in exercise tolerance, QOL, and depression. Exercise increased circulating immune cells (CD3+T, CD19+B, CD4+Th, CD8+T, CD56+NK, CD4+FOXP3+TRegs; p<0.05). CD16++CD14+ monocytes increased more than CD14++CD16- monocytes (p=0.001). Training did not adversely affect the immunophenotype response to incremental exercise Conclusions Exercise training was well tolerated in LHC patients and improves exercise tolerance QOL and depression symptoms. No adverse immunologic effects were identified.