Abstract
BACKGROUND: Isoniazid(INH) is an important first line drug in the management of active and latent TB. It?s widespread use and lack of diagnostic testing has resulted in increase in prevalence of Hr-TB, either alone or in combination with other drugs. katG and inhA mutations confer high and low level INH resistance respectively.
METHODS: Patients with Hr-TB were enrolled in a prospective observational cohort at a public tertiary care hospital in Aurangabad, India. Demographic characteristics, clinico-microbiological profile and treatment outcomes were noted (figure 1). Samples were analysed using line probe assays (LPA).Treatment was as per national policy guidelines.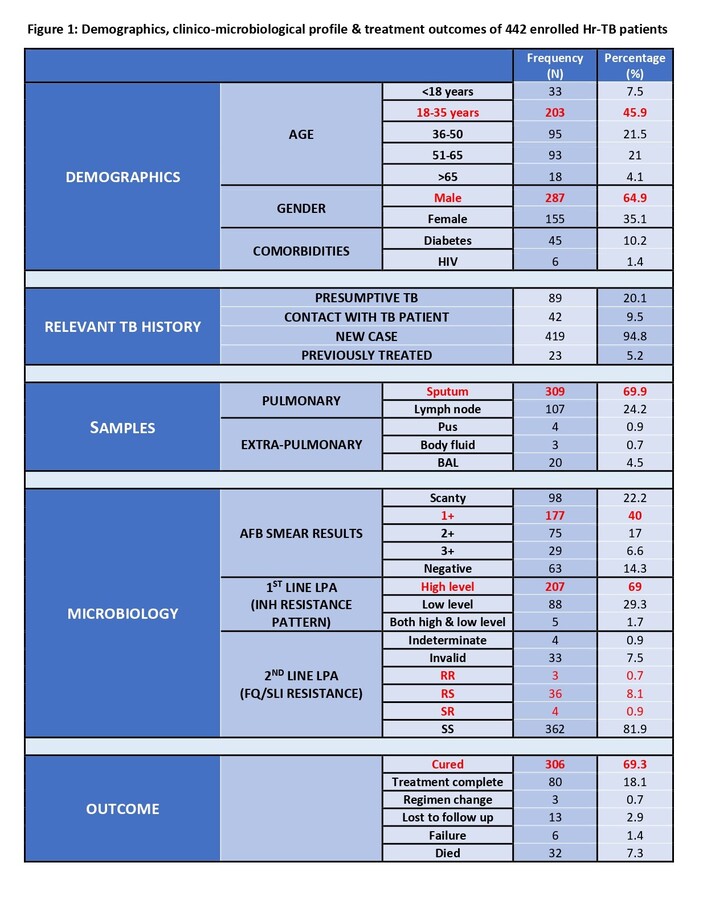
RESULTS: 442 patients were included with male predominance (64.9%). 53.4% patients were below 35 years. 1.4% had HIV confection and 10.2% were diabetic. Sputum samples were most common (69.9%) with 14.2% having a negative AFB smear. 69% patients had katG and 29.3% had inhA mutation. 9.7% patients had additional drug resistance on II line LPA (8.1% with FQ, 0.9% with SLI and 0.7% with both FQ & SLI). 69.3% were declared cured and 7.3% died. Outcomes were significantly worse in males(p=0.04) and with additional drug resistance(p=0.03). Age, mutation type, comorbidities did not affect treatment outcomes.
CONCLUSION: Hr-TB is frequently underdiagnosed and mismanaged leading to acquired drug resistance. LPA and universal DST should form integral part of TB program.