Abstract
Background
Patients with severe asthma appear to have low muscle mass, but the clinical consequences are unknown.
Aim
In a clinical sample of moderate to severe asthma patients, we aimed to assess muscle mass and strength and the association with functional and clinical outcomes.
Methods
Muscle mass and strength were assessed by the fat-free mass index (FFMI), 24h urinary creatinine excretion (CER), and handgrip strength test (HGS). Functional outcomes included pulmonary function and the 6-minute walking distance (6MWD), while the clinical outcomes included asthma control, quality of life and healthcare use.
Results
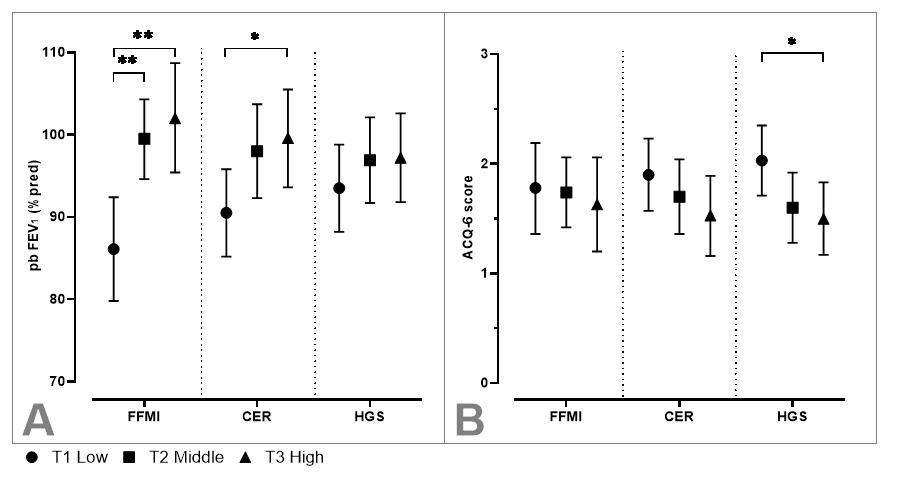
114 patients participated (36% male, mean±SD age 52±14 years, BMI 28±6 kg/m2). According to predefined criteria, 16% and 8% had low muscle mass defined by FFMI and CER respectively, which did not differ between GINA classes. Using multivariable regression analyses, both lower FFMI and CER were associated with lower values of FEV1 (Fig. A) and 6MWD, whereas a lower HGS was related to worse asthma control (Fig. B), poorer quality of life and a greater likelihood of emergency visits (all p<0.05).
Conclusion
This study shows that low muscle mass is prevalent in patients with moderate to severe asthma and, along with low muscle strength, is associated with worse clinical and functional outcomes. Our results encourage longitudinal studies into muscle function as a potential treatment target to improve asthma outcomes.