Abstract
Background
At the beginning of the COVID-19 pandemic, early intubation vs. oxygen therapy or additional non-invasive ventilation (NIV) was debated. Our centre followed a stepwise approach based on clinical judgement for therapy escalation from oxygen only up to extracorporeal membrane oxygenation (ECMO), rather than early or late intubation. We investigated the temporal development of non-pharmacological therapies of COVID-19 inpatients and correlations with patient survival.
Methods
This retrospective single-centre study on COVID-19 inpatients between March 2020 and December 2021 analysed anthropometric data, non-pharmacological maximum therapy and survival status.
Results
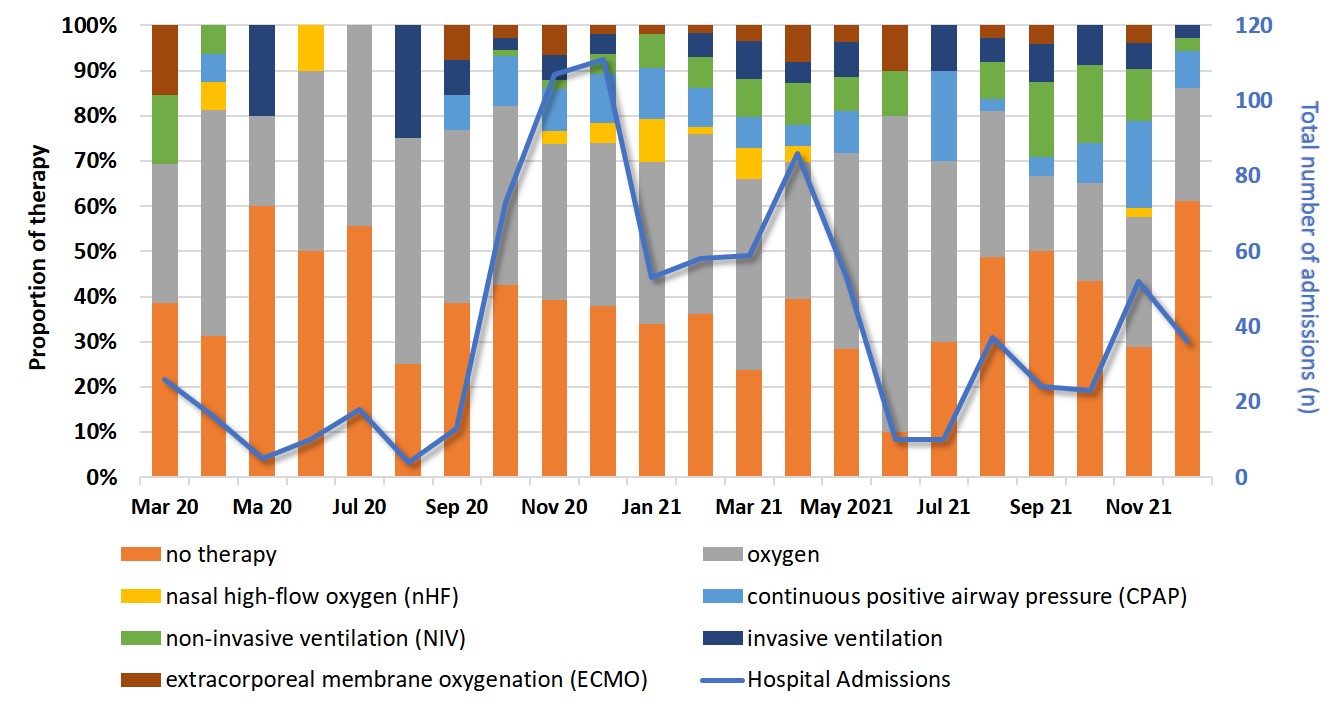
Of 836 patients (46% women), 106 (13%) died. Month-by-month analysis of the maximum therapies showed a stable distribution within the analysed period (Figure 1). Overall, 36% (n=303) had no therapy, 3% (n=21), high-flow oxygen (nHF), 9% (n=73) continuous positive airway pressure (CPAP), 7% (n=56) NIV, 4% (n=34) invasive ventilation and 4% (n=31) ECMO. Mortality rate in the invasively ventilated group was 74% and 6% in those treated with oxygen/nHF/CPAP/NIV.
Conclusion
The use of non-pharmacological therapy remained consistent throughout the studied period. The vast majority of patients could be treated without intubation. There are expected correlations between mortality and the escalation of the therapy modality due to disease severity.