Abstract
Background:
COVID-19 can lead to ARDS, a severe complication requiring invasive ventilation in the ICU. ARDS is characterized by protein-rich pulmonary oedema due to the alveolar-capillary barrier's hyperpermeability.
Aims:
This study aims to phenotype COVID-19 ARDS patients with variable amounts of pulmonary oedema using both biological and clinical markers.
Methods:
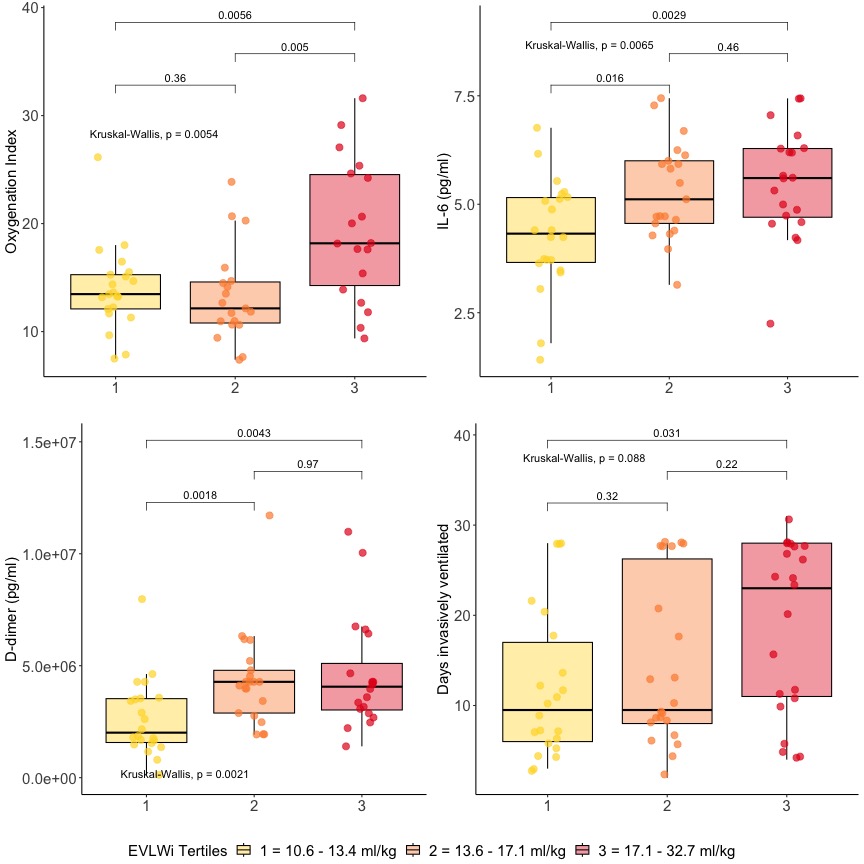
Transpulmonary thermodilution was used to measure extravascular lung water (EVLW) in 65 COVID-19 patients with ARDS. Patients were divided into tertiles based on the amount of EVLW at intubation, with cuts at 13.4 and 17.1 ml/kg. The groups were compared in terms of ICU admission conditions, ventilatory settings, serum biomarkers, and clinical outcomes.
Results:
Admission conditions were similar in the three EVLW groups. However, the highest tertile group had worse ventilatory and clinical outcomes, as demonstrated by a higher oxygenation index and higher number of ICU admission days (Table). Blood biomarkers also showed gradual worsening between the groups, with IL-6 and D-dimer showing the clearest differences (Figure).
Conclusion:
The amount of EVLW in COVID-19 ARDS relates to both biological and clinical variables. While biological differences can be identified in patients with intermediate EVLW, differences in clinical outcomes can only be seen in the highest tertile. These results help in the understanding of pathophysiological processes in COVID-19 ARDS.