Abstract
Acute Respiratory Distress Syndrome (ARDS) is a heterogeneous condition and can be classified into subphenotypes according to different inflammatory/clinical status. Identification of subpopulations may allow prognostic enrichment, although the time of analysis may change the classification according to response to treatment or disease evolution. We aimed to evaluate how may change the clustering of patients using data of baseline or day 3, and the prognosis of patients according to their evolution by changing or not the cluster.
Multicenter, observational of patients admitted to ICU due to COVID-19 infection. Clinical, physiological and biological data from 3739 patients ARDS receiving invasive mechanical ventilation were analyzed. Patients were grouped according to the k-prototypes algorithm using continuous and categorical data at baseline and day 3.
At baseline, 2265 (60%) patients were in cluster 1, the high mortality cluster characterized by higher SOFA scores and poor oxygenation. On day 3, the higher mortality cluster included 2021 (54%) patients (cluster 1). In addition, 699 (18%) patients switched from cluster 1 at baseline to cluster 2 at day 3, and 455 (12%) patients switched vice versa. Survival curves are shown in Figure 1.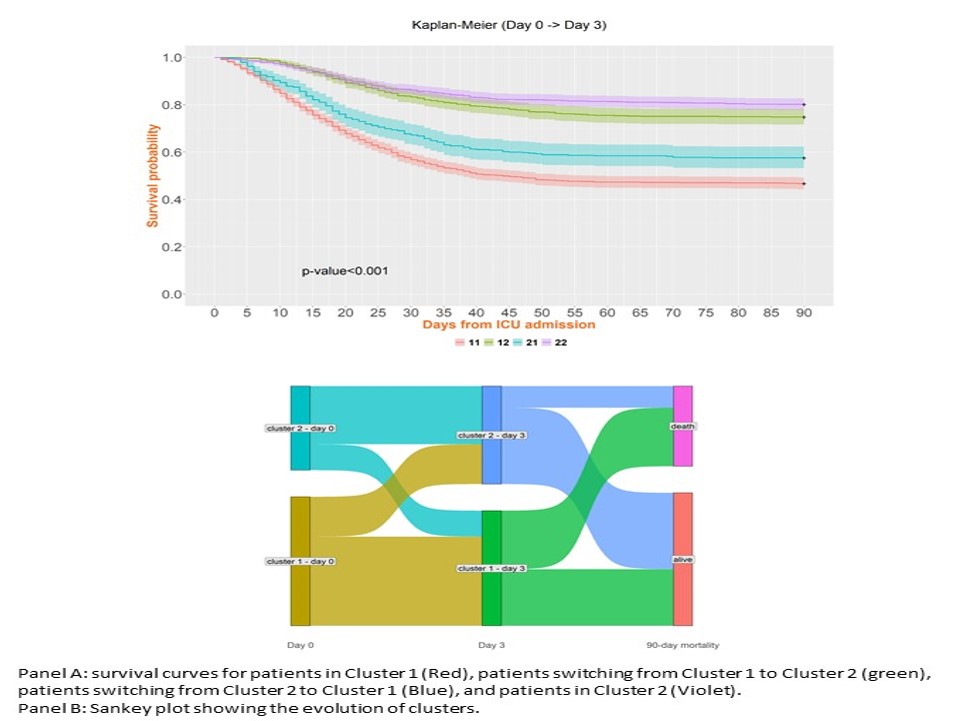
Patients may change their classification according to their evolution. This may improve or worsen their prognosis. For a better classification, the clustering must take into account the evolution of the patients.