Abstract
Introduction
Nutrition is a cornerstone care for all chronic respiratory diseases, there is still a gap in the literature regarding interstitial lung disease (ILD).
Objective
We aim to describe the nutritional status of our cohort and how this correlates with pulmonary functional test (PFT) and presence of UIP in CT
Methods
Retrospective cohort study. ILD patients who had nutrition evaluation from March 2021 to august 2022 were included(n=106). We collected PFT, CT pattern, symptoms and ILD cause. A licensed nutritionist collected weight, high, BMI, subjective global assessment(SGA) and arm strength with a grip dynamometer.
Results
Table 1: Cohort description. Fig 1: Correlation matrix.
| Age,yrs | 67 |
| Male(%) | 31(29,2) |
| Weight,Kg | 69,8 |
| BMI | 27,3 |
| SGA | A:77;B:26;C:3 |
| RA strenght(Kg) | 23,3 |
| LA strenght(Kg) | 22,2 |
| Dyspnea(%) | 75(70,7) |
| FVC, Lt | 2,23 |
| DLCO,ml/min/mmHg | 15,49 |
| Definitive UIP(%) | 28(26,4) |
| Time to PFT(months) | 3,29 |
| Time to CT(months) | 5,59 |
| ILD cause | |
| IPF(%) | 19(17,9) |
| CTD(%) | 52(49,1) |
| Others(%) | 5(33,1) |
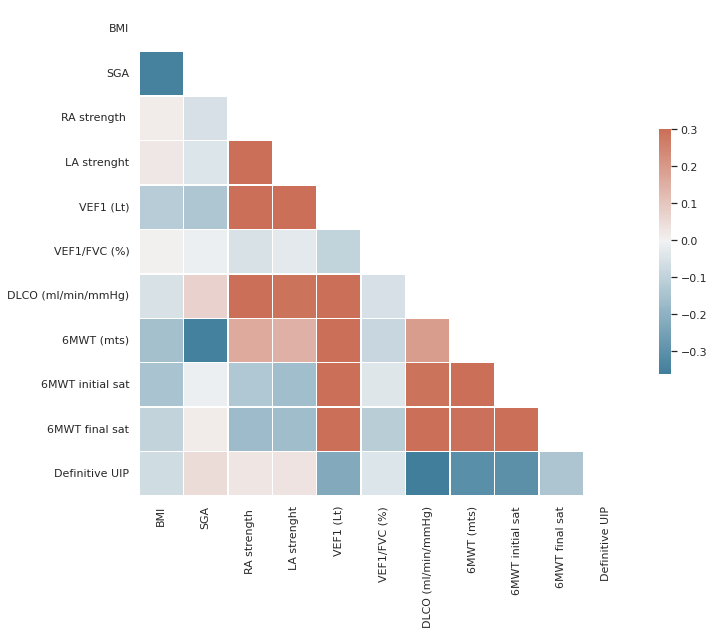
Grip strength has the best PFT correlation (FVC p=0,003;VEF1 p=0,002; DLCO p=0,006). SGA has the best negative correlation with meters in 6 minutes walking test(p=0,001)and performed slightly better than strength for UIP presence (Pearson correlation 0,12 vs 0,02).
Conclusion
Nutrition parameters correlates to patientīs respiratory status. To understand this relation will provide evidence to be applied specifically in ILD patientīs care.