Abstract
A study found 1 in 7 NHS workers are seeking work outside the NHS; more than at the height of COVID.2 Our RHCU provided level 2 care during the pandemic and saw a 54% mortality rate in the first year. Excessive workload, emotional pressure and being financially undervalued has left staff exhausted and demoralised. In our unit 41% of nurses and 29% of health care assistants (HCA) have since left. Frustrations are evidenced in the planned strikes.
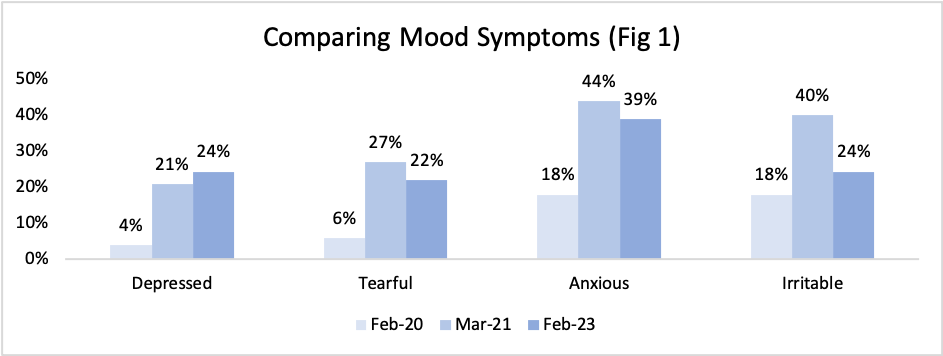
We reassessed the mental health and burnout of staff using Patient Health Questionnaire-9 and Oldenburg Burnout Inventory (OLBI). This was compared to surveys in Feb 20 and Mar 21.
50 questionnaires circulated; 82% return rate. Of which: 24% doctors, 32% nurses, 24% HCA and 20% other. 58% of staff had worked on RHCU for ?12 months. 32% of staff reported poor or fairly poor overall mental health rating, a 2.5x increase since Feb 20. 24% reported feeling depressed, 22% tearful, 39% anxious and 24% irritable, half the time or more (Fig 1).
95% had an OLBI score of medium or high, among which 50% of senior doctors scored high (>44/64). Staff who worked during February 20 (75%) were 2.3x more likely to have a high OLBI. 33% of junior doctors and 54% of nurses are unsure or would quit their job in current conditions.
Urgent support is needed to improve the well-being of our workforce.
2Weyman A. University of Bath. The new institute for Policy Research;Feb 23