Abstract
Introduction: Interstitial lung diseases (ILDs) are diverse disorders with varying prognoses. There is a growing interest in finding simple biomarkers to predict ILD outcomes. While most prior research has focused on IPF, more data is needed for prognostication in other ILDs.
Objective: Evaluating the differential blood count (DCBC) as a prognostic tool in ILDs.
Methods: A cohort of ILD patients who were diagnosed and followed-up from 2017 to 2022 at an expert ILD center was analyzed. The ability of DCBC parameters at ILD diagnosis to predict a composite outcome of mortality, lung transplantation or hospitalization for respiratory exacerbation was assessed.
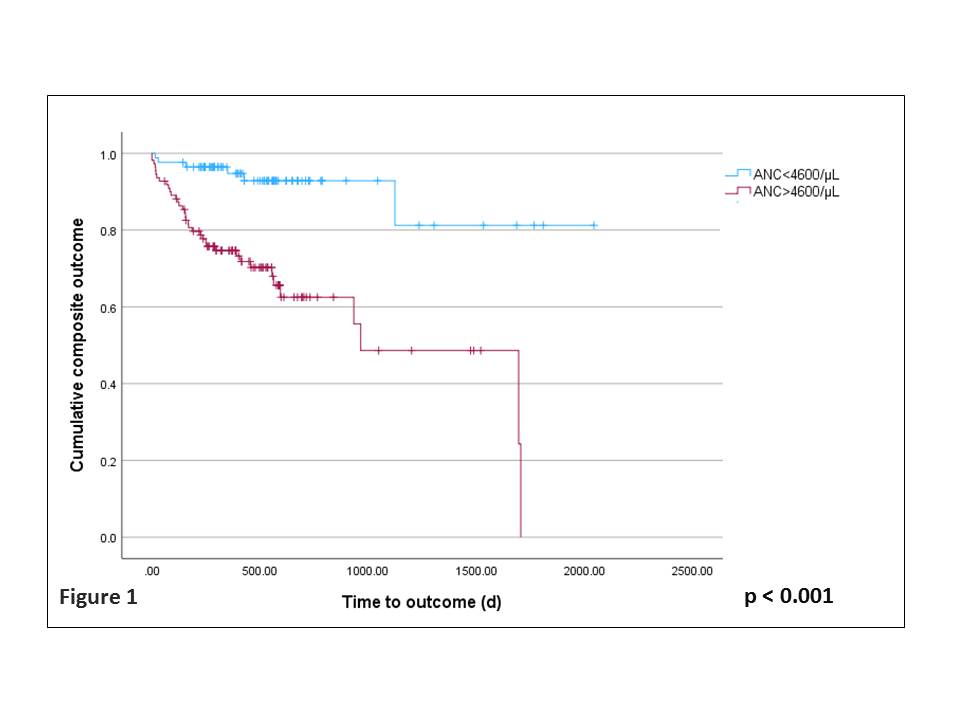
Results: 194 patients (54.1% males, mean age 64.5, 88.2% with non-IPF diagnoses) were included with a median follow-up of 426 days. Elevated absolute neutrophil count (ANC), monocytes, and platelets, as well as decreased hemoglobin and lymphocytes, were significant predictors of poor outcomes. After adjusting for age, gender, PFTs, ILD type and smoking history using multivariate analysis, only elevated ANC was found to be an independent predictor of poor prognosis. The optimal cutoff was determined as ANC above 4600/µL (adjusted HR = 5.3, 95% CI 2-13, p < 0.001, Figure 1). This was validated in an independent cohort of 193 ILD patients from another center (p = 0.006).
Conclusion: ANC greater than 4600/µL at ILD diagnosis is an independent predictor of poor outcomes in ILDs.