Abstract
Aim
This study aims to correlate quantitative chest CT (cCTs) scores with aetiology and severity of lung disease in bronchiectasis (BE) patients in the European Bronchiectasis Registry (EMBARC).
Methods
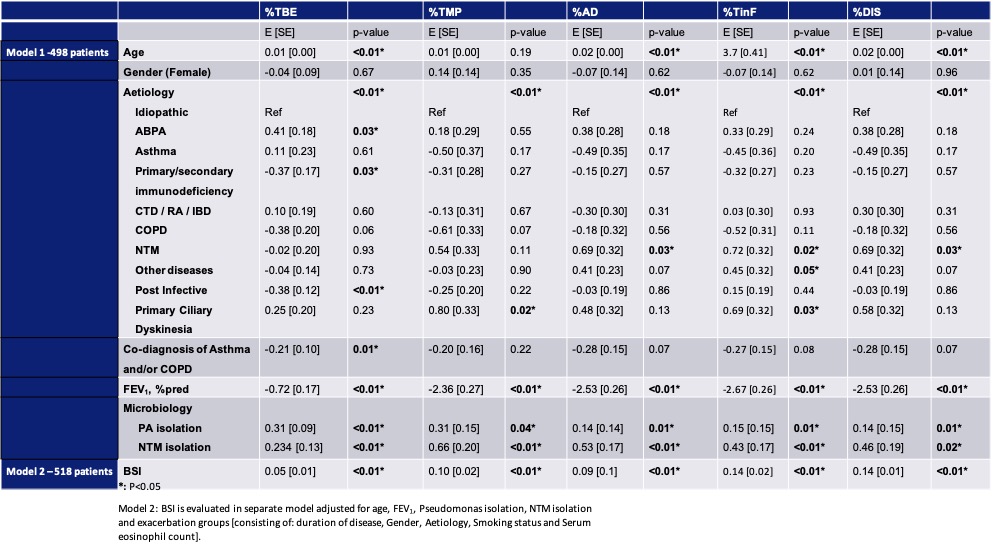
cCTs from EMBARC patients were analyzed semi-automatically using the validated Bronchiectasis Scoring Technique for CT (BEST-CT). BEST-CT scores are expressed as % of total lungvolume. Scoring items: consolidation/atelectasis (%ATCON), BE with and without mucus plugging (%BEMP, %BEwMP), airway wall thickening (%AWT), mucus plugging (%MP), ground-glass opacities (%GGO), emphysema/bullae(%EMPBUL), healthy airways and parenchyma (%HA, %HP). Composite scores were calculated: Total BE (%TBE = %BEMP + %BEwMP), total airway disease (%AD = %TBE + %MP + %AWT), total MP (%TMP = %BEMP + %MP), total inflammatory changes (%TinF = %ATCON + %BEMP +%MP) and total disease (%DIS = all but %HA & %HP). Composite scores vs clinical parameters were tested using multivariate linear regression.
Results
498 patients were included. PCD and NTM associated BE had more structural lung changes (SLC). Lower lung function, longer disease duration, higher severity scores, Pseudomonas (PsA) and NTM infection were independent predictors of more SLC (p<0.01 for each), while the number of exacerbations was not.
Conclusion
Lungfunction, aetiology, severity scores and PsA or NTM infection were most strongly correlated with the extent of SLC.