Abstract
Introduction: Home spirometry can deliver objective measures of progression and treatment response in interstitial lung disease (ILD). A structured home spirometry programme can be established involving clinician feedback; how patient experience evolves over time is unclear.
Aim: To examine how home spirometry use and understanding evolves in a real-world cohort within a UK ILD centre. To develop tools for patient-led home spirometry.
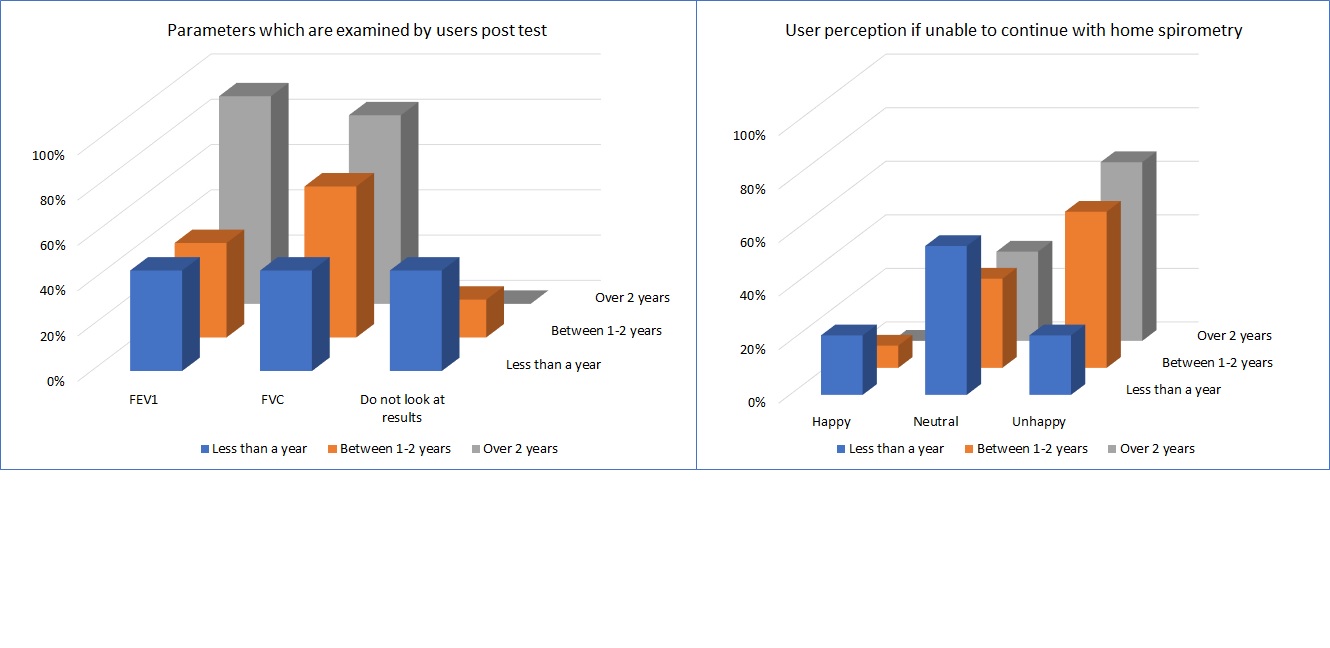
Methodology: Home spirometry was offered based on clinical need; training and standardised e-mail result feedback were provided. 35 users completed an online questionnaire, with an experience range of 32% (<1 year), 34% (1-2 years) and 34% (>2 years).
Results: Positive perception of spirometry increased with experience despite the majority considering it a reminder of their lung health. 71% of users undertook spirometry only when specified by clinician; 83% valued receipt of a standard reply. Awareness of results increased with experience but 92% described sending all data to clinicians as important. Only 25% found additional resources to support their own spirometry use.
Conclusion: Users viewed home spirometry as having value when accompanied by clinician feedback. Users showed little autonomy in using spirometry as an adjunct to self-management of their condition. This has resource implications for services implementing home spirometry programmes, which should be embedded within a self-management context.