Abstract
CPAP is the mainstream treatment for patients with OSA and was also used in the intensive care units during weaning from mechanical ventilation. It is controversial whether ventilation increased with increasing CPAP level based on indirect measurement of flow (e.g., RIP).
We used a custom-made apparatus to measure tidal volume (VT) at different CPAP levels (0, 5,10,15, and 20 cmH2O) in random order. The apparatus comprised a large plastic box with one end fixed to a full facemask which was in turn connected to a digital flow meter fixed inside the box (volume about 8 L) and the other end was connected to a CPAP with a tube. The pressure inside the box was monitored. VT was integrated from the flow signal (Figure 1).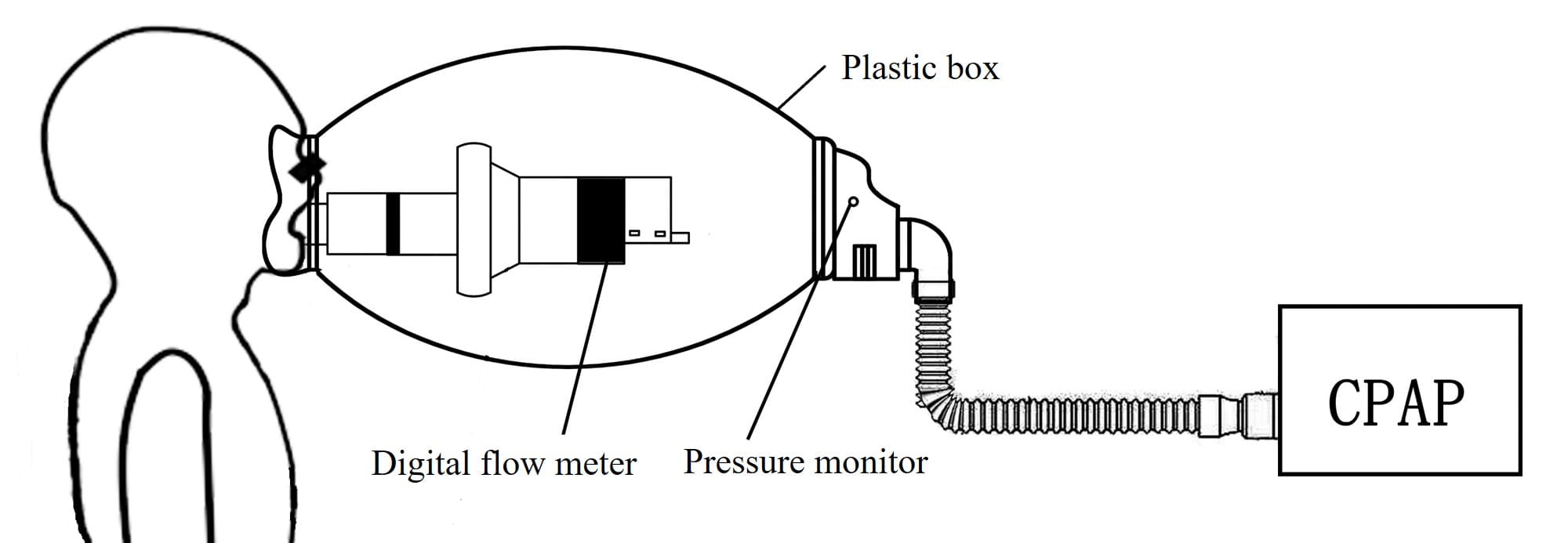
18 healthy subjects (age 30±8 Y, BMI 23.0±3.3 Kg/m2) were studied. Each level of CPAP was recorded for 5 minutes and there was a 3 minutes gap between different CPAP levels. The mean VT was 0.48±0.09 L, 0.48±0.10 L, 0.49±0.15 L, 0.50±0.12 L, and 0.48±0.10 L at 0, 5, 10, 15, and 20 cmH2O, respectively (p>0.05), with no statistically significant change in breathing frequency. There was no difference in minute ventilation (VE) between different pressure levels although VE increased with increasing CPAP and was 9.16±1.66 L, 9.27±1.86 L, 10.01±3.17 L, 9.73±2.43 L, and 10.02±2.68 L for 0, 5, 10, 15, and 20 cmH2O, respectively (p>0.05).
We concluded that CPAP has barely effect on ventilation although a large sample size study may be required.