Abstract
Goblet cell (GC) metaplasia is a paramount feature of small airway (SA) disease in COPD, often considered as present at all generations of SA. We aim to localize which generations of SA are affected by this process in a spectrum ranging from healthy and early-emphysematous to end-stage COPD lungs.
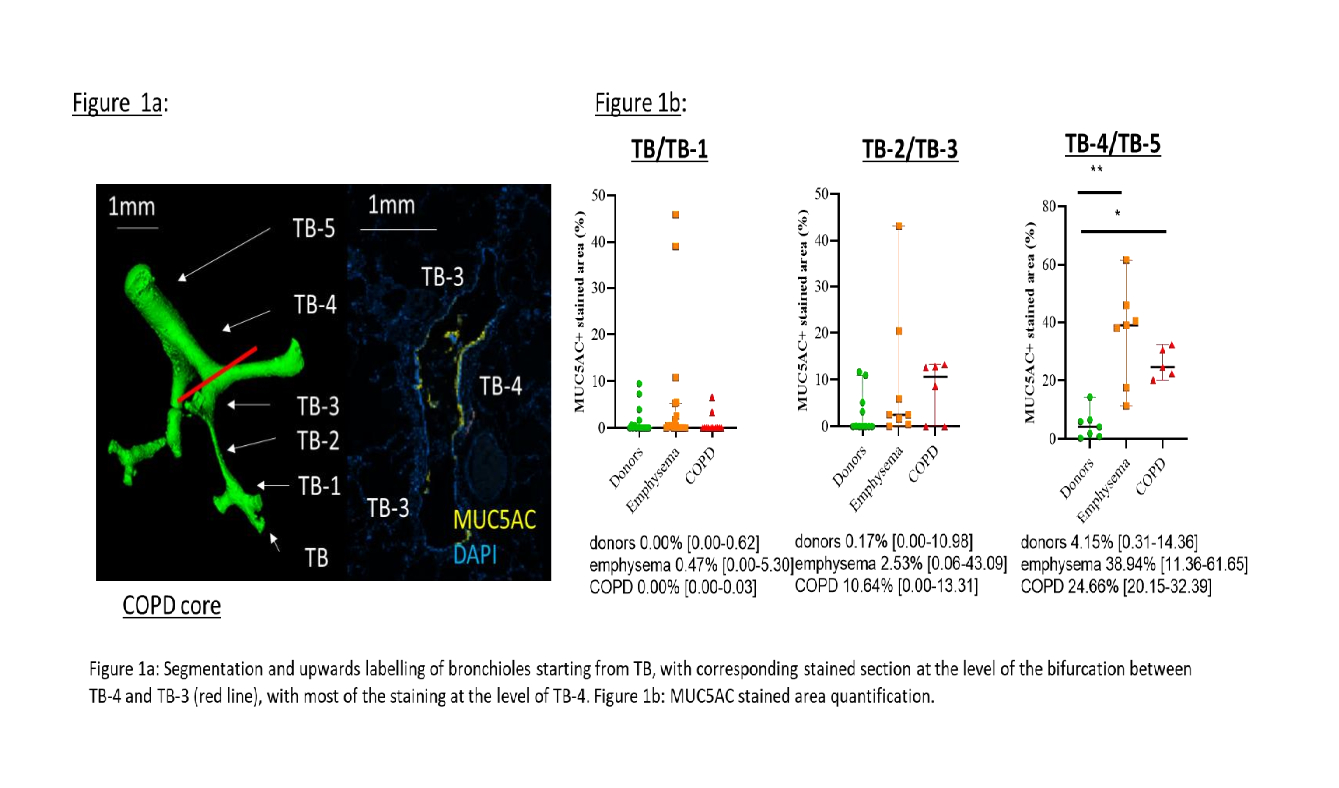
Donor lungs unused for extra pulmonary reasons (n=10), donor lungs radiologically and histologically characterized by emphysema (n=10) and COPD explants (n=10) were frozen at TLC and processed in cores (1.4 cm diameter cylinders). From each lung, up to 4 cores (27 donors, 20 emphysema, 15 COPD cores) were randomly selected and microCT-scanned (10?m resolution), and paraffin sections were stained for GC marker MUC5AC. SA were segmented on microCT and labelled as TB (terminal bronchioles)/TB-1, TB-2/TB-3 or TB-4/TB-5 according to the generation, upwards from TB (figure 1a).
At the level of TB/TB-1, MUC5AC stained area were low in all 3 groups. In TB-2/TB-3 airways, stained area was also low although more scattered in the emphysema group. At the level of TB-4/TB-5, MUC5AC was increased in emphysema (p= 0.019) and COPD (p=0.05) vs donors (figure 1b).
The data show that GC metaplasia occurs in the distal part of the SA from an early stage of the disease. However, the absence of GC metaplasia in the very distal airways needs to be taken into account when studying this vulnerable zone of the lung.