Abstract
Acute respiratory distress syndrome (ARDS) has no definitive pharmacological treatment (1) and Mesenchymal Stem Cells' (MSCs) extracellular vesicles (EVs) have been proposed as an innovative strategy (2).
The main objective is to study the effect of the MSCs' EVs on immune response in an acute lung injury (ALI) pre-clinical model, and how priming MSCs with lipopolysaccharide (LPS) can affect their therapeutic potential.
The ALI model was induced by the intratrcheal instillation of HCl and LPS. 9 h after, animals were administered with Control or LPS EVs, isolated from MSCs supernatant (normal and primed conditions). After 72 h, pro-inflammatory cytokines and chemoattractants expression was evaluated in lung tissue and bronchoalveolar lavage (BAL) macrophages. Differential and total cell count on BAL was analyzed by FACS.
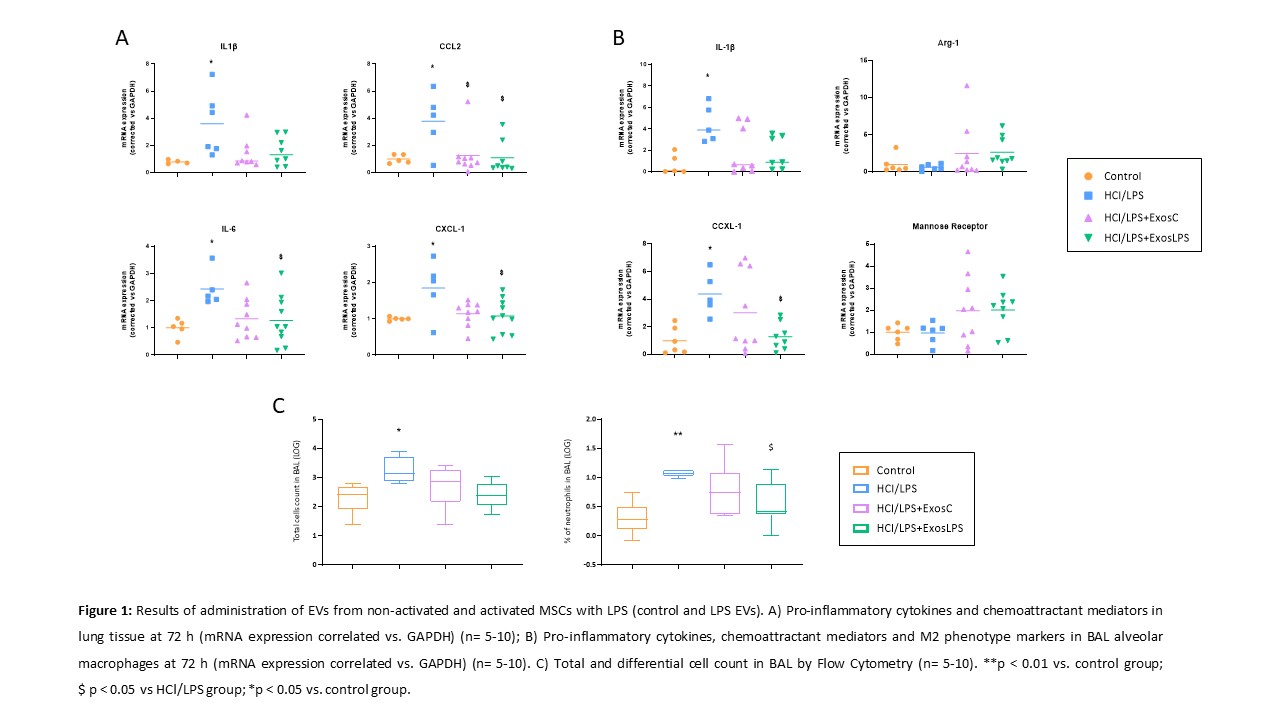
Control and LPS EVs reduced the expression of IL-1?, IL-6, CCL2 and CXCL-1 in lung tissue (Fig. 1 A, B), as well as, in the macrophages from BAL, which in addition, showed an increased expression of M2 phenotype markers (MR and Arg-1) compared to non-treated animals (Fig. 1 B). However, only rats that were treated with LPS EVs exhibited a significant reduction of infiltrated neutrophils in the intraalveolar space (Fig. 1 C).
MSCs-derived EVs reduce lung inflammation in an ALI model, and it is enhanced when MSCs are primed with LPS, by decreasing intraalveolar neutrophil infiltration.