Abstract
Aims
Subclinical heart failure may lead to congestion in the pulmonary veins and increased mortality. Aim: To determine the association of pulmonary vein volume with all-cause mortality in smokers with and without COPD.
Methods
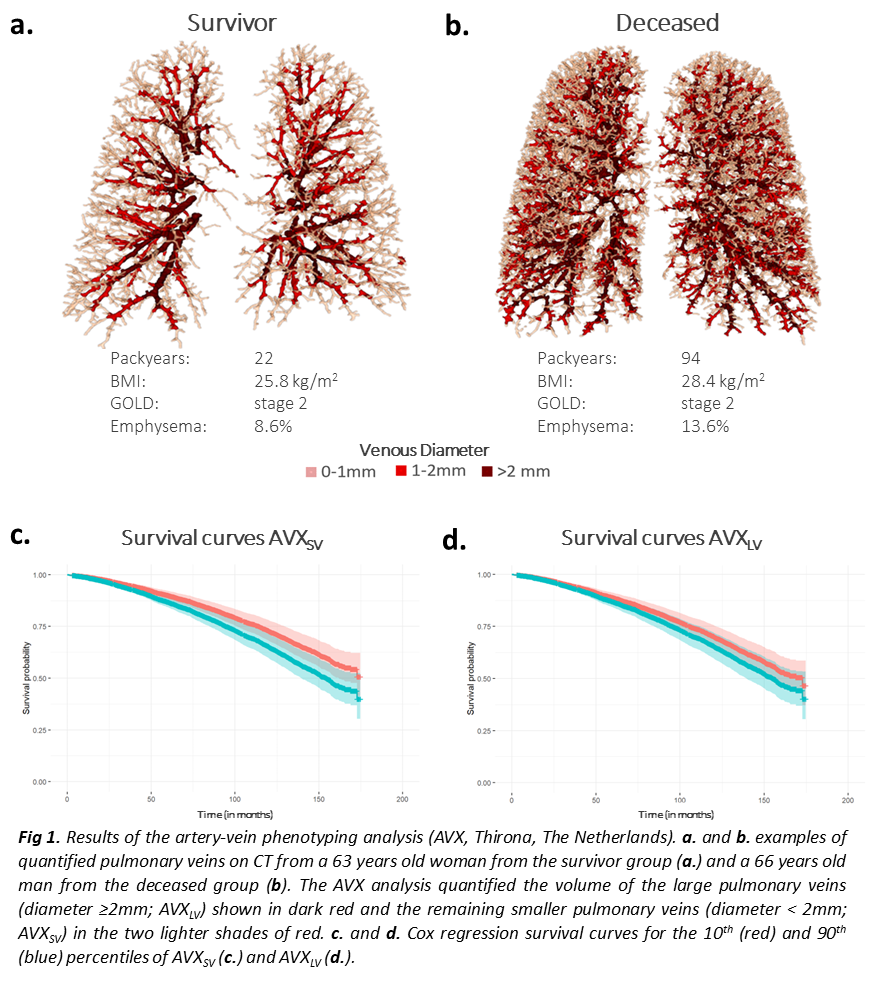
The artery-vein phenotyping analysis (AVX) was performed using the AI-based lung quantification platform LungQ (Thirona, The Netherlands). AVX quantified total volume of small (diameter <2mm; AVXSV) and large (?2mm; AVXLV) pulmonary veins on CT in 7903 participants of the COPDGene study, normalized for body height. Cox regression analysis was used to analyze associations between AVXSV and AVXLV scores and mortality. Corrections were made for age, sex, BMI, FEV1%predicted, mMRC, 6MWT, smoking status, emphysema, airway wall thickness, coronary artery calcium score, severe exacerbations, and scanner model.
Results
Mean age was 60.1±9.0 years; 3594 (45.5%) subjects had COPD. AVXSV was 82.3±13.3 mm3/cm; AVXLV 178.2±53.1 mm3/cm. Higher AVXSV and AVXLV were both associated with higher mortality, HR 1.57 (CI 1.31-1.88) and HR 1.07 (CI 1.01-1.13) per 50 mm3/cm, respectively.
Conclusions
Increased pulmonary venous volume is associated with a higher mortality in smokers with and without COPD, independent of emphysema and coronary artery calcium score, and may be a marker of volume redistribution as a result of heart failure.