Abstract
Current pharmacological treatment of idiopathic pulmonary fibrosis (IPF) consists of antifibrotics. Disease progression is in part monitored by pulmonary function tests (PFT). We aimed to assess the prognostic role of short-term PFT response to antifibrotics.
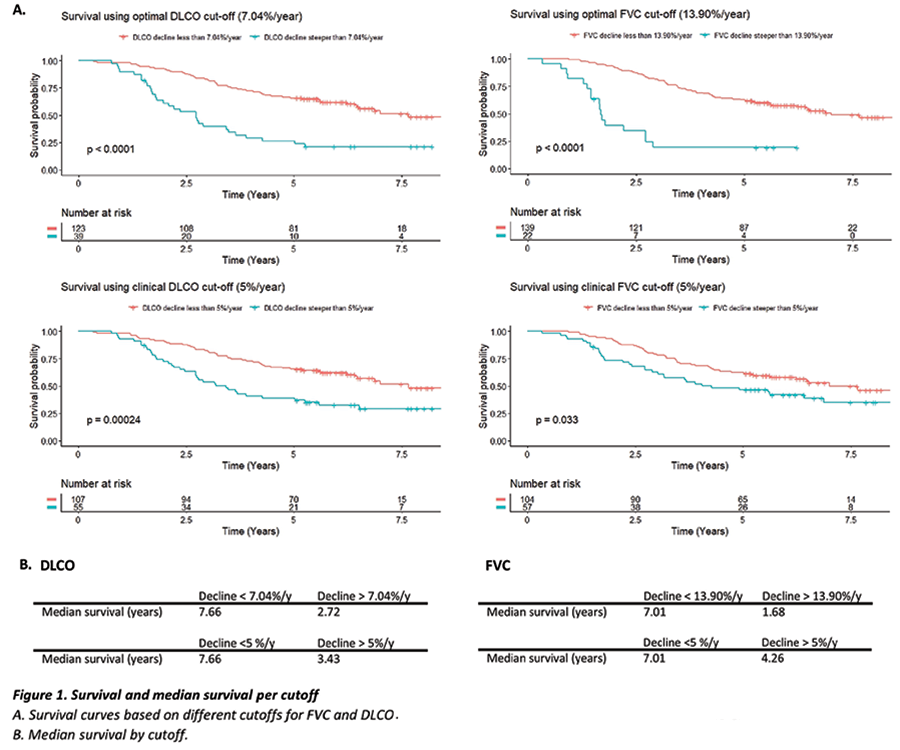
We quantified individual slopes per year using linear regression for functional vital capacity (FVC%pred) and diffusion capacity (DLCO%pred) evolution in the 18 months after the start of antifibrotics. Cox Proportional Hazards models were used to associate FVC%pred and DLCO%pred evolution (corrected for baseline disease extent, gender, and age) with survival. Optimal cutoffs were determined by Maximally Selected Rank Statistics. Survival curves and Logrank-tests were computed for these cut-offs and a clinical cut-off of 5% decline.
We retrospectively collected the data of 162 patients (PFT=733, 77.8% male, 2012-2016). Median age at antifibrotic initiation was 72.3y. Median overall survival after initiation of antifibrotics was 6.42y. 95.7% received pirfenidone, 4.3% nintedanib. Greater DLCO decline (per %, p <0.001, HR=1.03) and greater FVC decline (per %, p= <0.001, HR=1.05) were associated with increased risk of death or transplantation. Survival curves and optimal cutoffs are shown in figure 1.
To conclude, both steeper DLCO and FVC decline in the year after antifibrotic initiation were associated with higher mortality and could be used as a prognostic factor.