Abstract
Rationale: The GOLD 2023 report categorises patients without spirometric evidence of airflow obstruction but with respiratory symptoms or structural/functional abnormalities as Pre-COPD or Preserved Ratio with Impaired Spirometry (PRISm) (GOLD 2023 Report. https://goldcopd.org/2023-gold-report-2/. Accessed Feb 6, 2023). Data on outcomes in these patients are sparse.
Aims: To describe FEV1 changes and mortality over 3 years in patients with physician-diagnosed COPD in NOVELTY, recruited from primary and tertiary clinics.
Methods: Patients were classed as COPD, Pre-COPD or PRISm by spirometric GOLD criteria. Absolute mean±SD change in FEV1 from baseline to Year 3 is shown. Kaplan?Meier and the Cox model were used to estimate mortality.
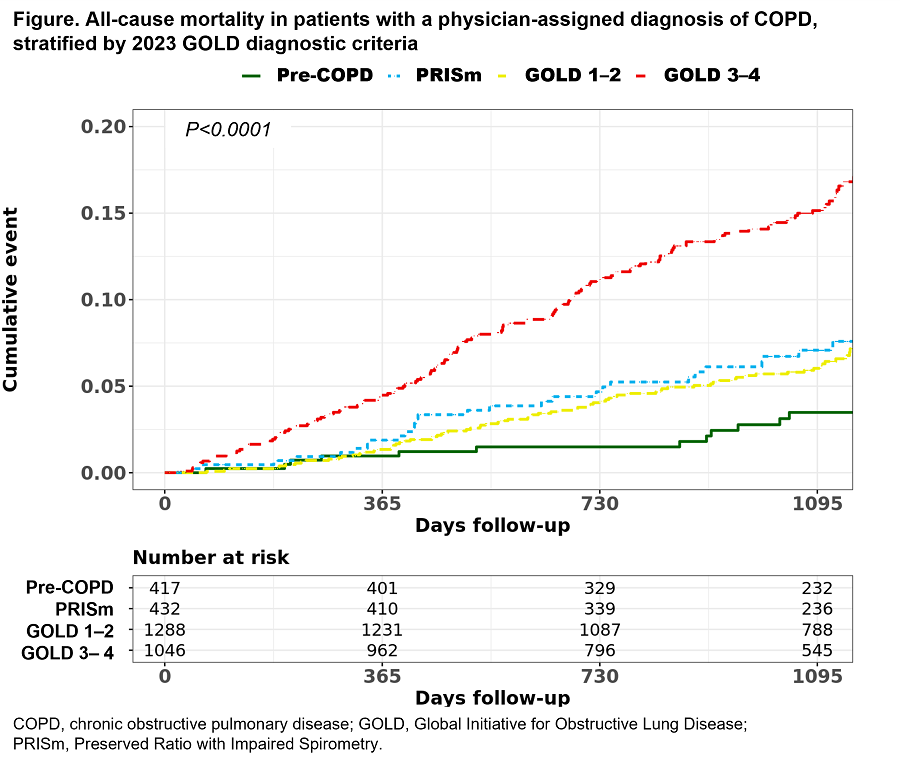
Results: In total, 3183 patients had physician-diagnosed COPD at baseline; 1197 had FEV1 data at Year 3. FEV1 change was greatest in Pre-COPD (?80±128 mL/yr; N=150; age=63±12 yr) and GOLD 1?2 (?53±91 mL/yr; N=535; age=68±9 yr), and smallest in PRISm (?14±107 mL/yr; N=161; age=63±10 yr) and GOLD 3?4 (?23±88 mL/yr; N=351; age=68±8 yr). At Year 3, mortality was highest in GOLD 3?4 and lowest in Pre-COPD (Figure). The age-adjusted hazard ratio for mortality for PRISm vs Pre-COPD was 2.5 (95% CI: 1.3?4.9).
Conclusions: Among physician-diagnosed patients, lung function decline in Pre-COPD vs GOLD1?2 and mortality in PRISm vs GOLD1?2 was similar, demonstrating heterogeneity consistent with the clinical diagnosis of COPD.