Abstract
Background:
The restrictive phenotype of chronic lung allograft dysfunction (CLAD), restrictive allograft syndrome (RAS), remains a major cause of mortality after lung transplantation. As per current ISHLT consensus, a patient is only diagnosed with CLAD if FEV1 declines ? 20% from baseline. However, patients may demonstrate clear, chronic interstitial changes on subsequent CTs, without significant FEV1 decline. There are no clear guidelines on management of this subgroup of patients, yet they may evolve to true RAS with longer follow-up.
Methods:
Patients transplanted at our center 2010-2021 (n=789) were phenotyped per ISHLT consensus, leading to inclusion of n=69 RAS patients. Impact of pre-CLAD opacities on FEV1 was assessed in a linear mixed model. Impact on Kaplan-Meier survival estimates was assessed with log-rank test.
Results:
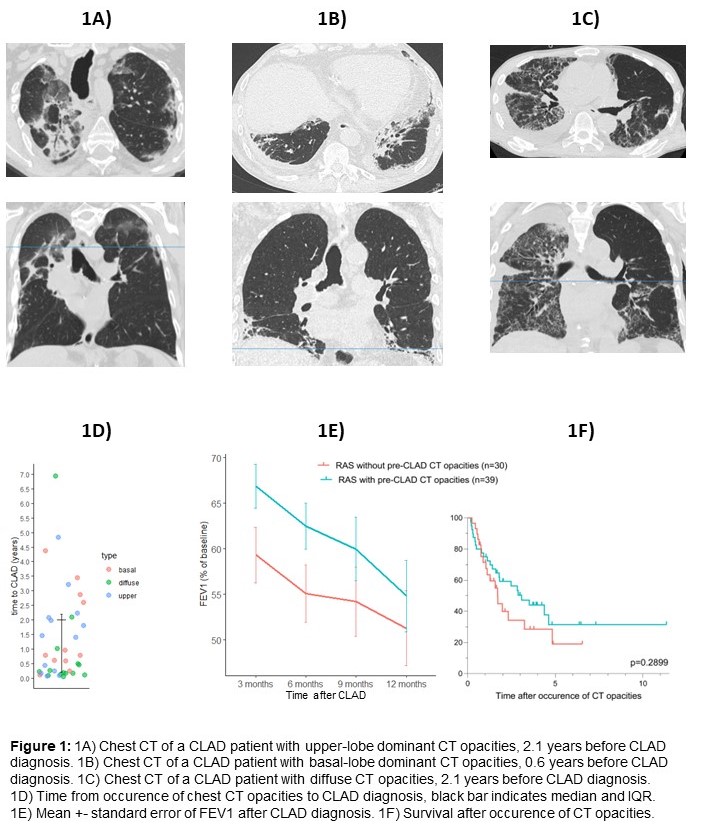
57% of RAS patients (n=39) demonstrated CT opacities prior to CLAD diagnosis. Time to CLAD diagnosis was highly variable and not significantly impacted by localization of infiltrates (figure 1D). FEV1 after CLAD in patients with pre-CLAD opacities was significantly higher compared to those without pre-CLAD opacities (p=0.023, Figure 1E). Survival after occurrence of CT opacities was similar compared to true RAS patients (Figure 1F).
Conclusion:
Incorporating routine CT imaging during follow-up in the current guidelines could help to better detect allograft dysfunction at an earlier stage.