Abstract
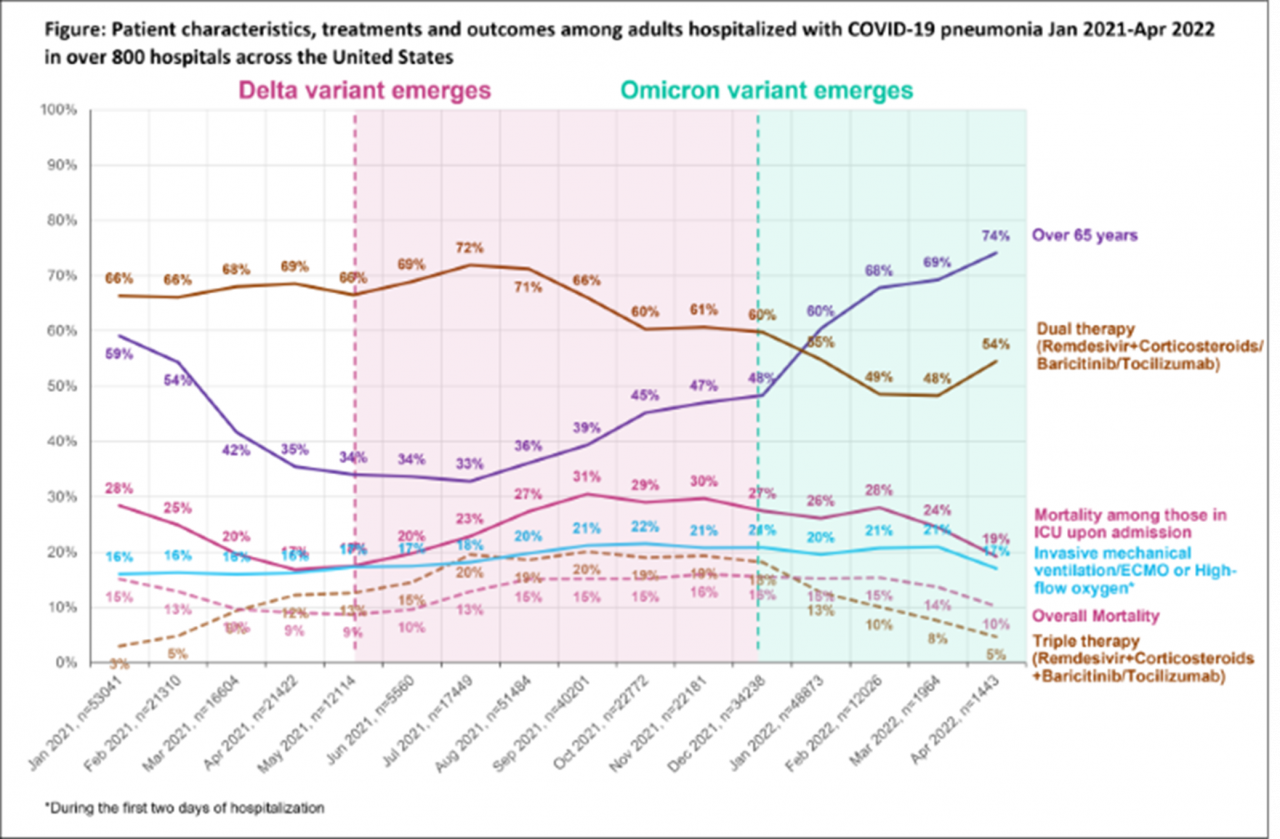
This is a retrospective study of adult patients hospitalized with primary diagnosis of COVID-19 and secondary diagnosis of pneumonia due to COVID-19 between Jan'21-Apr'22 in the Premier Healthcare Database. Patient characteristics, severity, treatments and outcomes were examined during circulating variants of concern: pre-Delta, Delta and Omicron.
382,682 patients were hospitalized for COVID-19 and pneumonia due to COVID-19 in 844 hospitals: median age 63 yrs (IQR:52-74), 72% white, 48% female.
Compared to pre-Delta, patients during Delta period were younger (median age 60 vs 65; p<.0001), had fewer comorbidities (p<.0001), higher oxygen requirements upon admission (20% vs 16% on IMV/ECMO or high-flow; p<.0001), more likely to be treated with triple therapy (Remdesivir+Corticosteroids+Baricitinib/Tocilizumab, 19% vs 6%; p<.0001) and higher mortality rates (14% vs 13%; p<.0001).
Compared to Delta, patients during Omicron period were older (median age 67 vs 60; p<.0001), had more comorbidities (p<.0001), similar oxygen requirements of IMV/ECMO or high-flow upon admission, less likely to be treated with COVID-19 therapy (p<.0001) but higher mortality rates (15% vs 14%; p<.0001).
A subgroup (n=68,028; Jan'21-Apr'22) requiring ICU on admission had a mortality rate of 26%.
With the changing dominant variants, COVID-19 patient characteristics and outcomes have evolved significantly.