Abstract
Cough impacts up to 98% of people with chronic respiratory diseases (CRD) and about 50% of pulmonary rehabilitation (PR) attendees. PR shows promise in enhancing cough-related quality of life (CR-QoL), yet the determinants for responsiveness, i.e., reaching clinically significant improvements, in this domain are unclear. We explored determinants of responsiveness in CR-QoL with PR in people with CRD.
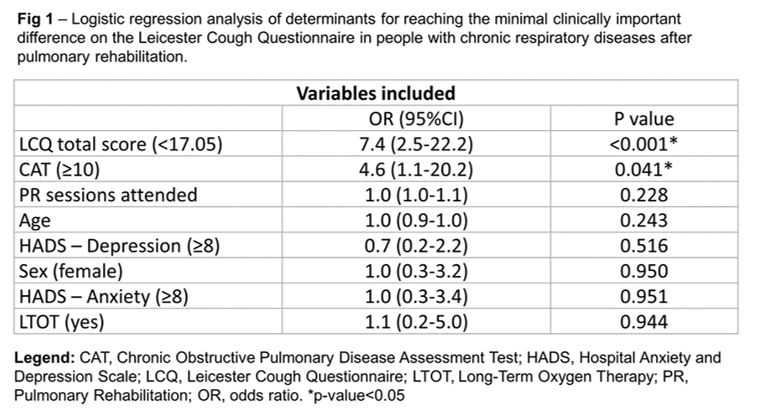
This retrospective study included adults with stable CRD who completed a 12-week PR program. Potential determinants were chosen based on literature and included age, sex, long-term oxygen therapy, the COPD Assessment Test (CAT), the Hospital Anxiety and Depression Scale and the Leicester Cough Questionnaire (LCQ). Achieving the minimal clinical important difference (MCID) of ?1.3 points on the LCQ total score confirmed a clinically significant response. Logistic regression was used to explore the contribution of the selected determinants to reach the MCID.
111 subjects (33%?, 69±10years, 60% COPD) attended 88[74-96]% of PR sessions. Individuals with low CR-QoL (LCQ<17.05) or those with medium or higher disease impact (CAT?10) were 7.2 and 4.6 times more likely to reach the MCID for the LCQ after PR, respectively (Fig 1).
Exhibiting low CR-QoL or a medium or higher disease impact at baseline are determinants for improving CR-QoL with PR. Further studies should explore cough as a treatable trait in PR and strategies for those who do not respond to PR.