Authors: Rachel Ong-Salvador and Kevin De Soomer
Overview
Spirometry is a diagnostic test used to aid in the diagnosis of lung diseases and monitoring lung health. This physiological test measures how an individual inhales or exhales volumes of air as a function of time. The primary signal measured in spirometry is either volume or flow.
In order to perform the test properly, it is essential to know which parameters are measured during the test and how this relates to lung physiology. This module will provide definition and illustration of the different parameters measured during spirometry. The procedure of measurement will be discussed in Module 4: How to perform the procedure including reading and reporting of results.
Aims
- To provide the basic definition of the terms used in spirometry
- To illustrate the different parameters used in spirometry
- To describe the characteristics of a flow-volume curve
- To describe the characteristics of a volume-time curve
Definition of terms
Spirometry indices:
ATPS: ambient temperature and pressure, saturated; denoting a volume of gas saturated with water vapor at ambient temperature and barometric pressure.
BTPS: body temperature and pressure, saturated; denoting a volume of gas saturated with water vapor at 37°C / 99°F and ambient barometric pressure.
Spirometry devices measure lung function in ATPS conditions. Since ambient temperature differs from body temperature, the measured results need to be converted to BTPS so that the measured value reflects the conditions within the patient's lung. All volumes and capacities are expressed in litres at BTPS.
Correction factor: In spirometry, the term correction factor refers to the correction factor which is needed to convert values measured from one set of conditions to another set of conditions.
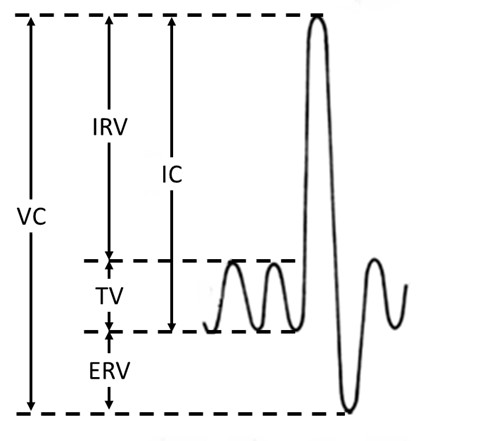
Figure 1: Vital Capacity (VC)
Vital Capacity (VC): The volume change measured at the mouth between a full inspiration and full expiration (Figure 1).
The vital capacity is subdivided into the tidal volume (TV), inspiratory reserve volume (IRV) and expiratory reserve volume (ERV) (Figure 1).
Tidal Volume (TV): The volume of air which is inhaled or exhaled during a respiratory cycle (normal breathing). This is a dynamic lung volume that can vary depending on the level of physical activity (Figure 1).
Inspiratory Reserve Volume (IRV): The maximum volume of air that can be inhaled from the mean end inspiratory level (Figure 1).
Expiratory Reserve Volume (ERV): The maximum volume of air that can be exhaled from the level of the functional residual capacity (FRC) (Figure 1).
Inspiratory Capacity (IC): The volume of air that is inhaled from FRC, to a position of maximum inspiration (Figure 1).
The slow VC can be derived either as a inspiratory (IVC) or expiratory maneuver (EVC) (Figure 2).
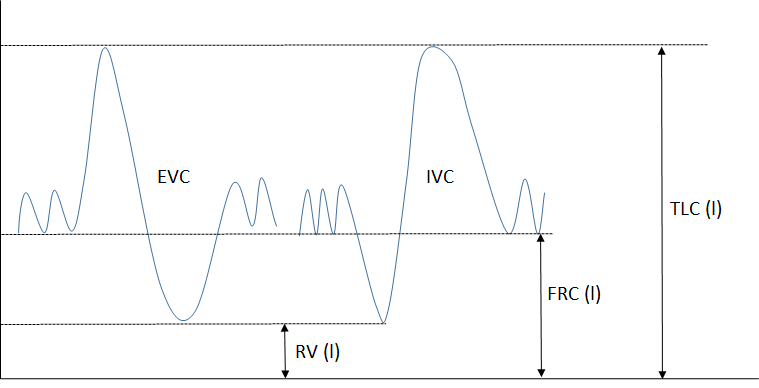
Figure 2: Expiratory Vital Capacity (EVC) and Inspiratory Vital Capacity (IVC)
Expiratory Vital Capacity (EVC): The vital capacity measured during an expiratory manoeuvre. Starting from end-tidal volume, the subject inhales fully and subsequently exhales maximally until plateau is reached (Figure 2).
Inspiratory Vital Capacity (IVC): The vital capacity measured during an inspiratory manoeuvre. Starting from end-tidal volume, the subject exhales maximally until a plateau is reached then inhales fully (Figure 2).
The following three parameters fall under static lung volumes and are not measured during spirometry. These parameters were included in this module to provide the participant a complete parameter list of lung volumes and capacities.
Residual Volume (RV): The volume of gas remaining in the lungs after a full exhalation (Figure 2).
Functional Residual Capacity (FRC): The volume of gas present in the lungs after a normal expiration, is mainly determined by the interaction between elastic recoil of the chest and lungs (Figure 2).
Total lung capacity (TLC): The volume of gas contained in the lungs after a full inhalation (Figure 2).
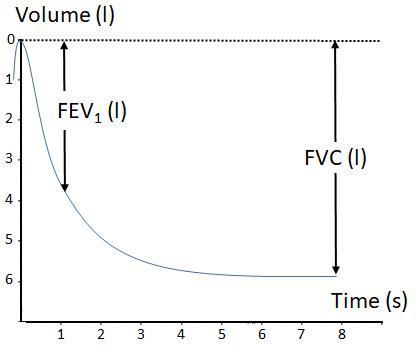
Figure 3: Volume-time curve
Forced Inspiratory Vital Capacity (FIVC): The volume of air that is forcefully inhaled after the FVC manoeuvre.
Forced Expiratory Volume in 1 second (FEV1): The FEV1 is the volume of air that is forcefully exhaled in the first second during the FVC manoeuvre. FEV1 is an index used for assessing the severity of airway obstruction, bronchoconstriction or bronchodilation (Figure 3).
FEV1/(F)VC ratio: The FEV1 expressed as a percentage of the (F)VC is the standard index for assessing and quantifying airflow limitation. This parameter is reported as a decimal fraction to two decimal places.
As IVC > EVC > FVC in patients with obstructive lung disease, the VC should be specified when using the FEV1/VC ratio, hence FEV1%FVC (forced expiratory ratio, FER) or FEV1%IVC. The Tiffeneau-index is FEV1/IVC.
Forced inspiratory volume in 1 second (FIV1): The FIV1 is the volume of air that can be forcefully inhaled in the first second during a forced inspiratory manoeuvre following the FVC manoeuvre.
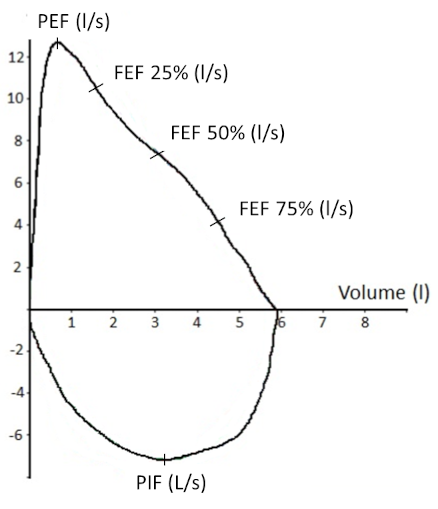
Figure 4: Flow-volume curve
Peak Expiratory Flow (PEF): The highest expiratory flow achieved during the FVC manoeuvre which is started without hesitation. This parameter is commonly expressed in litres per second (Figure 4).
Peak Inspiratory Flow (PIF): The highest inspiratory flow achieved during the FIVC manoeuvre which is started without hesitation. This parameter can be expressed in litres per second or litres per minute (Figure 4).
Forced Expiratory Flow 25-75% (FEF 25-75%): The mean forced expiratory flow between 25% and 75% of the FVC. This index is taken from the flow-volume curve with the largest sum of FEV1 and FVC. It is highly dependent on the validity of the FVC measurement and the level of expiratory effort (Figure 4).
Diagnostics:
Lung volume: refers to the volume of gas within the lungs.
Lung capacity: refers to the volume of air which comprises two or more lung volumes.
Reversibility testing: Reversibility testing is usually performed for the diagnosis of asthma. Spirometry is performed, after which a bronchodilator is given that can either be a short-acting β-agonist or other agents, such as anticholinergics.
Bronchodilator responsiveness testing is a determination of the degree of improvement of airflow in response to bronchodilator administration as measured by changes in FEV1 and FVC.
End of forced expiration (EOFE): Previous standards used the term "end of test" and the abbreviation "EOT" to denote end of forced expiration (EOFE). These standards stress the importance of a maximal inspiration after the forced expiration. As such, the end of forced expiration is not the end of the manoeuvre, and hence the term EOFE is used.
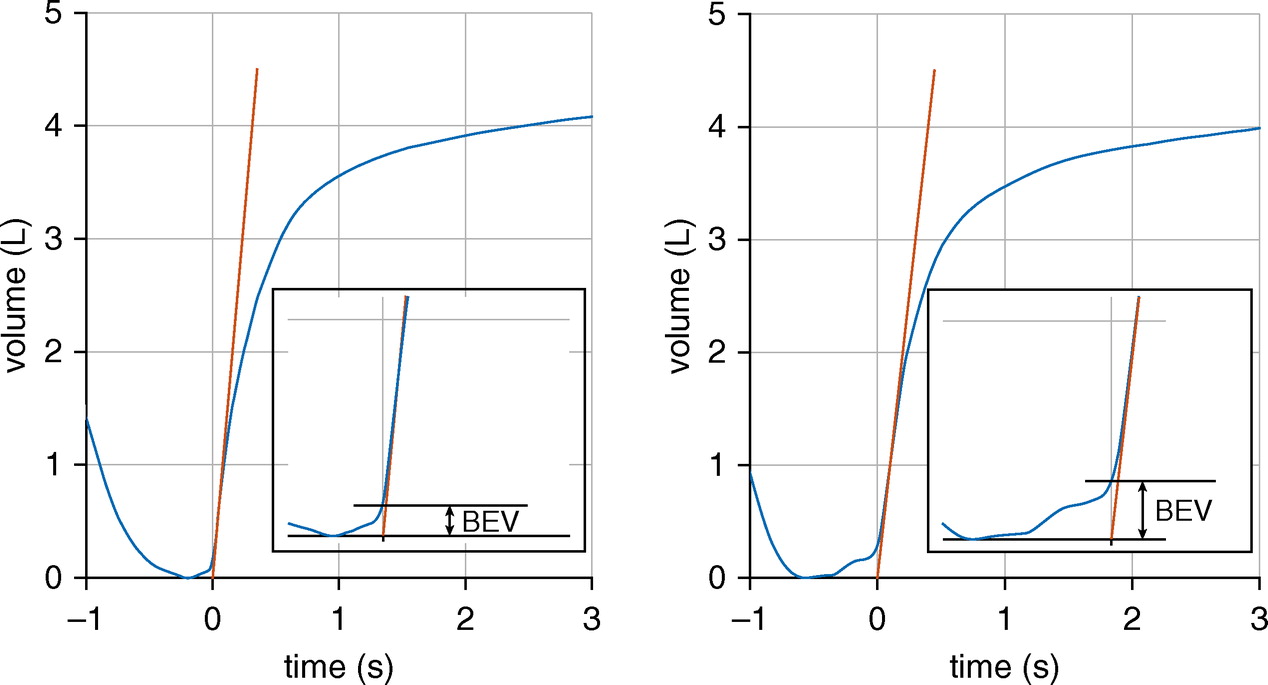
Figure 5: Back-extrapolation [1]
Back-extrapolation (BEV): The volume of air measured before the start of the FVC manoeuvre (Figure 5).
If a patient is slow to start the expiratory manoeuvre, the measure can be corrected by back extrapolation. Time zero can be assessed by visual analysis, and should be reported.
- Most computerised spirometers correct automatically.
- If the machine does not have a printout, it can be difficult to assess quality of manoeuvre.
